The first CRISPR treatment for diseases was approved by the MHRA, UK on 16th November, 2023. Following a thorough evaluation of its safety, efficacy, and quality, the Medicines and Healthcare Products Regulatory Agency (MHRA) has approved a novel medication for patients 12 years of age and older with sickle-cell disease and transfusion-dependent β-thalassemia.
Casgevy is the first approved medication that uses the ground-breaking CRISPR gene-editing technique, for which its creators were given the 2020 Nobel Prize. The approval by the Medicines and Healthcare Products Regulatory Agency (MHRA) was based on acceptable clinical trial results. the technology for the trials was developed by Vertex Pharmaceuticals Inc. and CRISPR Therapeutics AG.
Sickle cell disease and β-thalassemia are hereditary disorders resulting from mutations in the genes for haemoglobin, which red blood cells utilise to transport oxygen throughout the body. The genetic error which can cause sickle cell anaemia can cause severe pain and life-threatening illness.
Mechanism of Casgevy
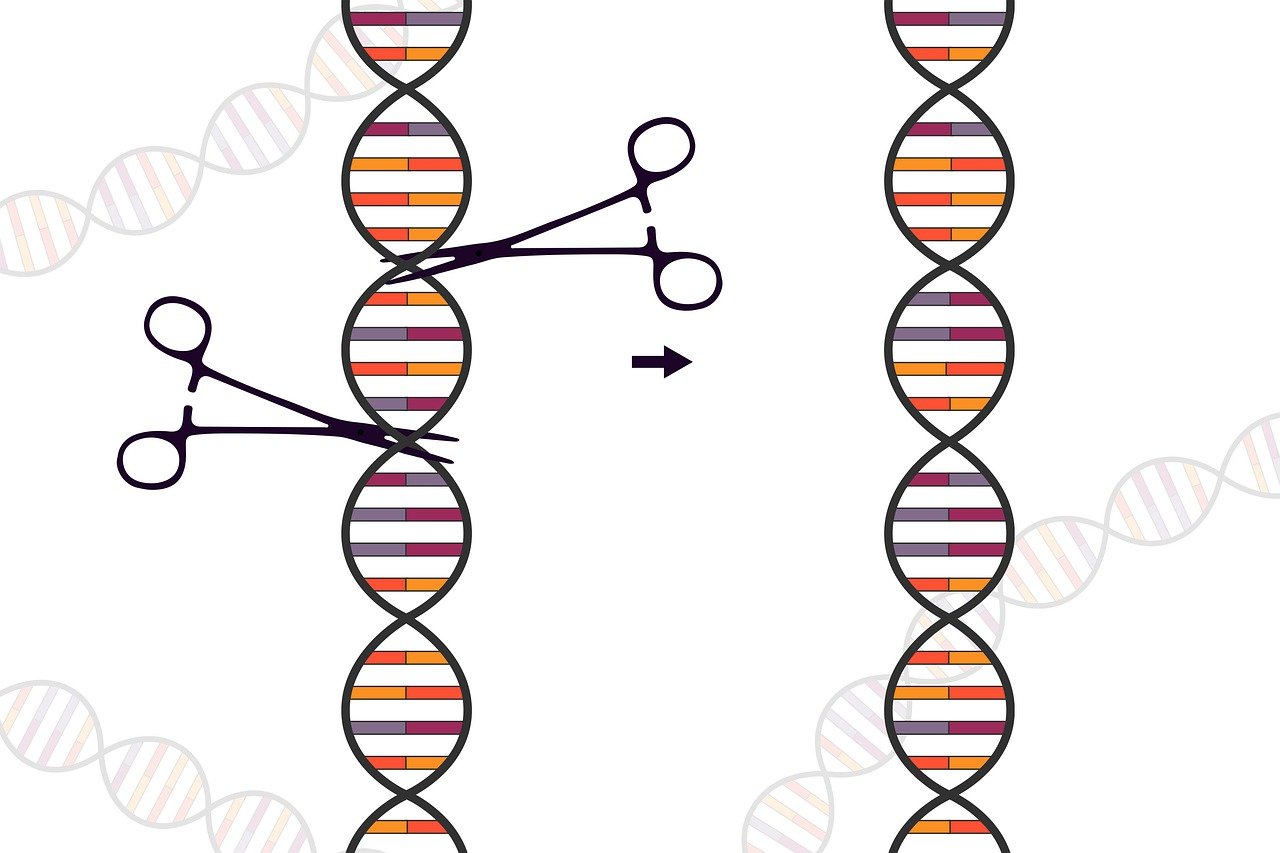
Casgevy’s mechanism of action involves correcting the defective gene in a patient’s bone marrow stem cells, enabling the body to create healthy haemoglobin. This is accomplished by extracting stem cells from the patient’s bone marrow, altering them in a lab, and then reinfusing them back into the body. The effects of this procedure might last a lifetime.
Trial Results
Based on the data in MHRA’s Press release.
In the clinical trial for sickle-cell disease, 45 patients have currently received Casgevy but only 29 patients have been in the trial long enough to be eligible for the primary efficacy interim analysis. Of these eligible patients, 28 (97%) were free of severe pain crises for at least 12 months after treatment.
In the clinical trial for transfusion-dependent β-thalassemia, 54 patients have currently received Casgevy but only 42 patients have been in the trial long enough to be eligible for the primary efficacy interim analysis. Of these, 39 (93%) did not need a red blood cell transfusion for at least 12 months after treatment. The remaining three had more than a 70% reduction in the need for red cell transfusions.
Side effects from treatment were similar to those associated with autologous (from a person’s own cells) stem cell transplants, including (but not limited to) nausea, fatigue, fever and increased risk of infection.
No significant safety concerns were identified during the trials. Safety continues to be closely monitored by the MHRA and the manufacturer.
Both trials are ongoing and further results will be made available in due course.
Also read| Researchers developed gel-mediated cancer drug delivery for solid tumors
Comments
Both sickle cell disease and β-thalassemia are painful, life-long conditions that in some cases can be fatal. To date, a bone marrow transplant – which must come from a closely matched donor and carries a risk of rejection – has been the only permanent treatment option.
The MHRA will continue to closely monitor the safety and effectiveness of Casgevy, through real-world safety data and post-authorisation safety studies being carried out by the manufacturer.
I would like to thank the patients with lived experiences who engaged with us as part of the assessment process and gave us valuable insight into their lives and the challenges of managing their condition.
Julian Beach, Interim Executive Director of Healthcare Quality and Access at the MHRA
Sickle cell disorder is an incredibly debilitating condition, causing significant pain for the people who live with it and potentially leading to early mortality.
There are limited medicines currently available to patients, so I welcome today’s news that a new treatment has been judged safe and effective, which has the potential to significantly improve the quality of life for so many.
John James OBE, Chief Executive of the Sickle Cell Society
Nobel Prize 2020 in Chemistry
The CRISPR/Cas9 genetic scissors are one of the most useful tools in gene technology, according to Emmanuelle Charpentier and Jennifer A. Doudna. With the help of these, scientists may precisely alter the DNA of plants, animals, and microbes. This technique may fulfil the hope of treating genetic disorders and has had a revolutionary effect on the life sciences. It is also helping to develop novel cancer treatments.
Source: MHRA Press release
Report: Achuth B S
Last updated:
Graduated from the University of Kerala with B.Sc. Botany and Biotechnology. M.Sc. Biotechnology from the University of Kerala. Attended certificate course in Artificial Intelligence for Everyone from Deeplearning.AI, Influenza Prevention and Control from World Health Organization. Attended workshops related to Bioinformatics at the University of Kerala. 3 years of experience in website management. Experience in WordPress, Blogger, Google Analytics, and Google Search Console.