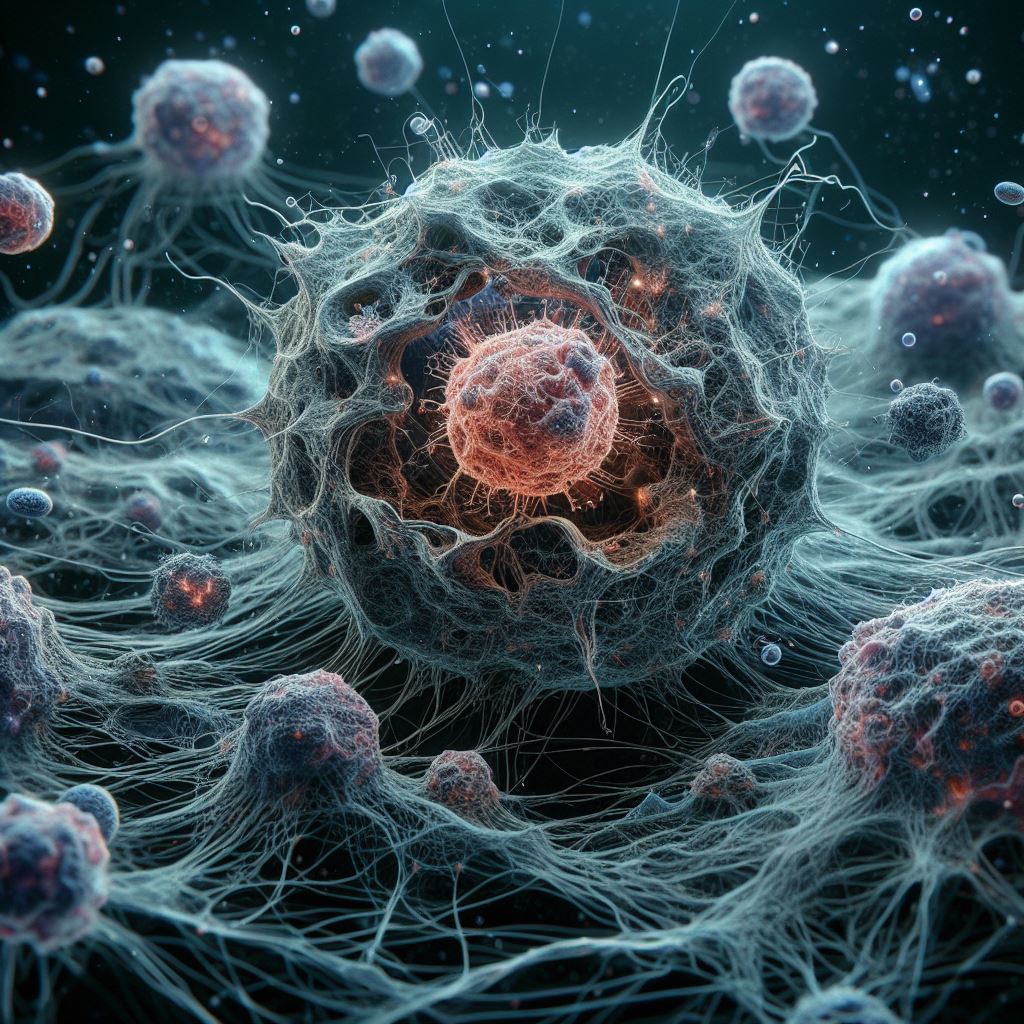
A new study may provide the answer to why myeloid leukemias relapse after chemotherapy has mostly eliminated cancerous cells and how repurposed medications might inhibit proliferation.
A subpopulation of leukemic stem cells (LSCs) that do not increase and are thus not destroyed by chemotherapy can be seen in the bone marrow of AML patients. After receiving therapy, these cells do, however, begin to increase and become AML cells, albeit it is unknown what initiates this process.
Researchers from the Princess Maxima Centre of Paediatric Oncology, Newcastle University, and the University of Birmingham examined single cells from patients with t(8;21) Acute Myeloid Leukemia, a particular kind of blood cancer, to find out what caused the uncommon LSCs to proliferate. Their work was published in Nature Communications.
Leukemic stem cells normally seem asleep which is why they are not killed by chemotherapy, but we reasoned that something must trigger them to start growing in order for the leukaemia to come back.
These cells are very rare and difficult to study but by examining gene expression in single LSCs we found genes being expressed that encode for growth regulators normally not present in myeloid cells. Both cell types are found in the bone marrow alongside the AML cells, but healthy stem cells do not respond to their signals. By aberrantly upregulating these growth regulators, leukaemic stem cells now can respond to growth factors that are present in the body and tell them to grow.
Professor Constanze Bonifer
Preventing the development of undesired stem cells
The VEGF signalling receptor, KDR, which is generally only expressed in blood vessels, and the IL-5 receptor, which is normally only expressed in eosinophils, were the growth regulators found in this investigation. Furthermore, the leukaemia produced VEGFA, the growth factor that binds to KDR, suggesting that it can promote its development. After identifying these receptors, the scientists verified that they could stimulate the formation of stem cells by turning them on in a lab setting. Crucially, they also demonstrated how repurposing medications against VEGF (Avastin, licenced for a variety of solid tumours, including colorectal cancer) and IL-5 signalling (Fasenra, approved for eosinophilic asthma) may limit growth in a dish and mice.
An exciting result from these studies is the fact that the expression of these receptors is specific to this particular type of leukemia. They are expressed as a result of the presence of a specific disease-causing mutation giving rise to the onco-fusion protein RUNX1::ETO which reprograms the gene regulatory network that defines how a cell responds to outside growth signals.
This work highlights the power of single cell analysis for digging deep into what regulates the growth of AML cells. It also highlights the fact that AML sub-types may have to be treated as a separate entities.
Professor Olaf Heidenreich
Also Read| Breast cancer screening will become fast, affordable, and accurate with a hand-held biosensor
We were very excited to find not one but two new, and potentially druggable targets to prevent relapse in these patients. Being told your cancer has come back is devastating news and we want to prevent this happening. Unfortunately, as these receptors were so specific this would only work for t(8;21) acute myeloid leukaemia and is not a magic bullet.
However, inspection of other single cell data from different leukemia sub-types show that other growth regulatory pathways are upregulated in their stem cell population as well. We are now hoping to find those that can be hit in other types of AML
Dr Sophie Kellaway
Blood cancer is the UK’s third biggest cancer killer and acute myeloid leukemia is a particularly aggressive form of blood cancer that can come back even after initial treatments have been successful.
This research uncovers why one specific type of acute myeloid leukaemia can return, and could lead to the development of new treatments with the potential to stop the cancer coming back, giving new hope to people affected by this specific form of leukaemia. However, further work is needed to see whether a similar approach could be taken for other forms of acute myeloid leukaemia and more broadly much more research is desperately needed to develop effective, kinder treatments for all blood cancers.
Dr Suzanne Rix
Also Read| Research: Genes that encode immunity are altered in Alzheimer’s patients blood
Source: University of Birmingham News
Journal Reference: Kellaway, Sophie G., et al. “Leukemic Stem Cells Activate Lineage Inappropriate Signalling Pathways to Promote Their Growth.” Nature Communications, vol. 15, no. 1, 2024, pp. 1-22, https://doi.org/10.1038/s41467-024-45691-4.
Last Modified