Regenerative medicine has the amazing potential to eliminate the need for donors for patients in the future who require fresh cells, tissues, or organs. For those in need of a transplant, safe, on-demand alternatives will take the place of organ shortages and cell type mismatches.
The difficult issue of persuading stem cells to develop into desirable cell types for treatment is one of the numerous obstacles this innovative science presently faces. Furthermore, immunological rejection poses a significant obstacle to the use of the appropriate cells or tissues, even if they are produced and are capable of performing their intended functions in the body. Today’s regenerative medicine treatments need systemic immunosuppression to get beyond this barrier, which leaves patients open to environmental threats including germs, viruses, and cancer cells.
Researchers at the Medical University of South Carolina and the University of Florida recently worked together to develop a novel, highly specific method of treating type 1 diabetes (T1D) that addresses these challenges by utilizing a tagged beta cell transplant in conjunction with localized immune protection from specialized immune cells that are also tagged with a complementary but inert targeting molecule.
One of the study’s lead scientists, Leonardo Ferreira, Ph.D., a researcher at MUSC Hollings Cancer Center, said that combining stem cell engineering with regulatory T cell (Treg) engineering was the first step toward an easily accessible, off-the-shelf treatment for type 1 diabetes.
Their findings were published in the journal Cell Reports.
The researchers detailed a novel partnership that combined the delicate surgical and chimeric antigen receptor (CAR) T cell expertise at Hollings with the beta cell engineering capabilities of Holger Russ’s lab, an associate professor of pharmacology and therapeutics at the University of Florida.
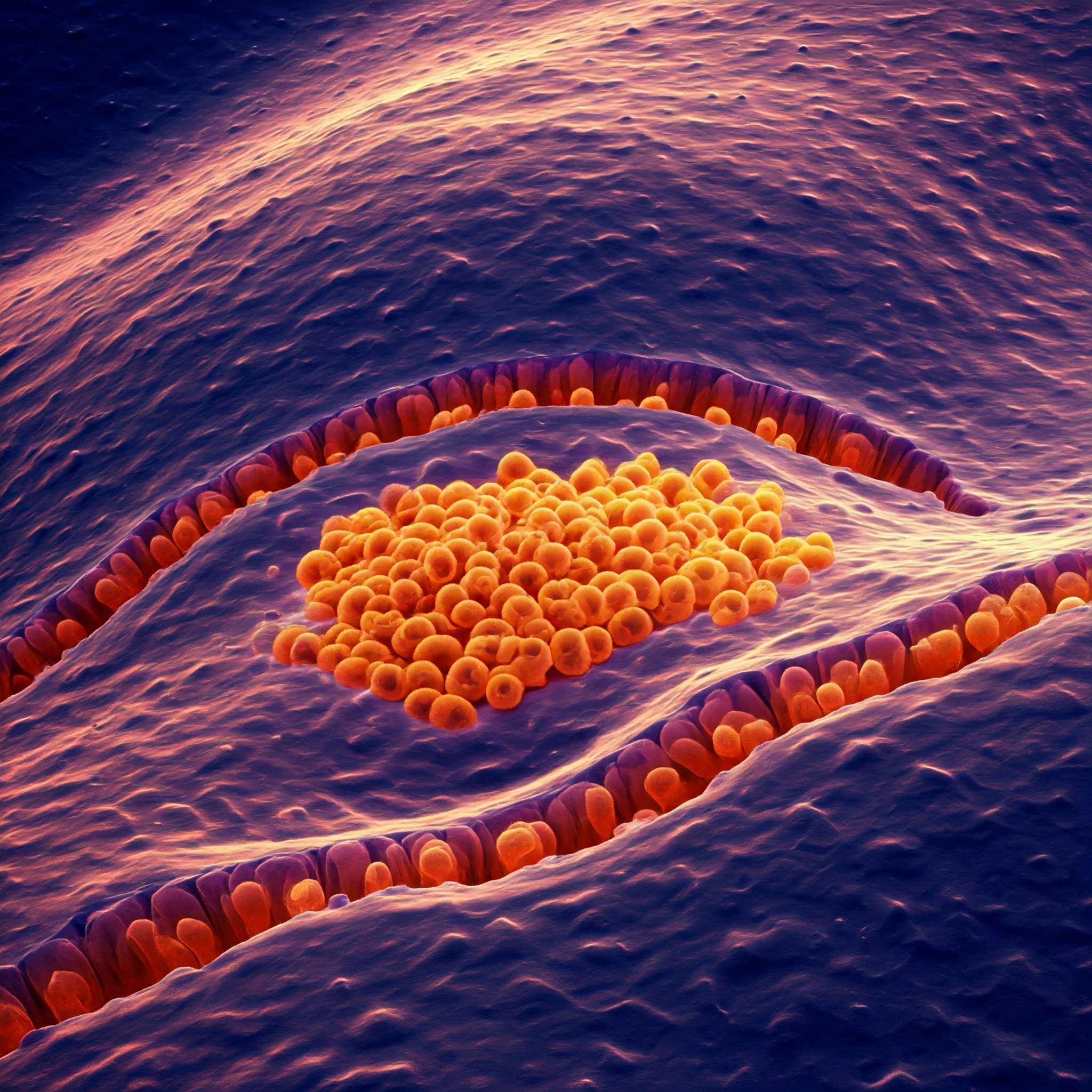
Pancreatic beta cells, which generate the hormone insulin to control blood sugar levels, are the target of an immune system self-attack in T1D patients. Patients are compelled to live with a high-maintenance routine of glucose monitoring and insulin control in order to preserve health and prevent serious problems including neuropathy, amputation, and blindness because they lack a dependable method of self-regulating blood glucose levels.
Most of the cells of the immune system are focused on killing invasive elements. But Tregs are the generals of the immune system. They make sure that nothing goes overboard, and they train the immune system on how to respond in the future.
Leonardo Ferreira, Ph.D.
For the time being, certain individuals with poorly managed type 1 diabetes could think about receiving an islet cell transplant utilizing donor beta cells. After being separated and purified from a donor pancreas, beta cells are sent to the patient’s liver so they may settle there and start secreting insulin. To prevent the body from rejecting the foreign beta cells, patients who choose this option must be immunosuppressed for the remainder of their lives. Additionally, donor cells must be available, which might mean lengthy wait times or not at all.
The researchers employed tagged beta cells made from stem cells as part of an engineering plan to concentrate on a different approach.
To test their approach, the researchers employed a mouse model. They demonstrated that the cells were integrated and started to produce functional insulin by introducing beta cells that were modified from stem cells and had a nonreactive tag, an inactivated form of the epidermal growth factor receptor, into the kidney capsules of immunocompromised mice. To assess the transplanted beta cells’ capacity to withstand a simulated immune response, the mice were subjected to an aggressive immune cell type in the next testing phase. As anticipated, the immune reaction destroyed every beta cell, which is also what occurs in T1D patients.
The researchers combined the immunological challenge with specific Tregs to prevent the killing response in the subsequent phase. A receptor that selectively detected the inactive EGFR tag on the transplanted beta cells was used to tag these cells utilizing CAR technology. After taking this extra precaution, the researchers saw that the transplanted beta cells were safe, healthy, and effective in their new environment, providing the immunological protection they had hoped for.
Also Read: Researchers developed lipid nanoparticles for netter mRNA therapies
Now that Ferreira and associates have demonstrated that their method of treating T1D is feasible, they intend to carry out more research, which will include creating a whole library of locks and keys—differentiated stem cells and tagged protective Tregs that can be used to treat a variety of conditions, including lupus, other autoimmune diseases, and some types of cancer.
There are still some unanswered problems, such which ligand is best for human transplantation and how long Treg-mediated immune protection lasts. The ligand or tag ought to be inert, meaning it shouldn’t interfere with the cells’ ability to operate or trigger any response that might have unintended consequences. Furthermore, it is yet unclear if a single Treg therapy would be successful or if it will need to be repeated at undetermined intervals. One therapy could be sufficient since Tregs can teach immune cells to sustain immunological tolerance, but further investigation is required to comprehend the long-term impacts fully.
Source: Hollings Cancer Center – News
Journal Reference: Barra JM, Robino RA, Castro-Gutierrez R, Proia J, Russ HA, Ferreira LMR. Combinatorial genetic engineering strategy for immune protection of stem cell-derived beta cells by chimeric antigen receptor regulatory T cells. Cell Rep. 2024 Nov 18;43(11):114994. DOI: 10.1016/j.celrep.2024.114994. Epub ahead of print. PMID: 39561045.
Last Modified: