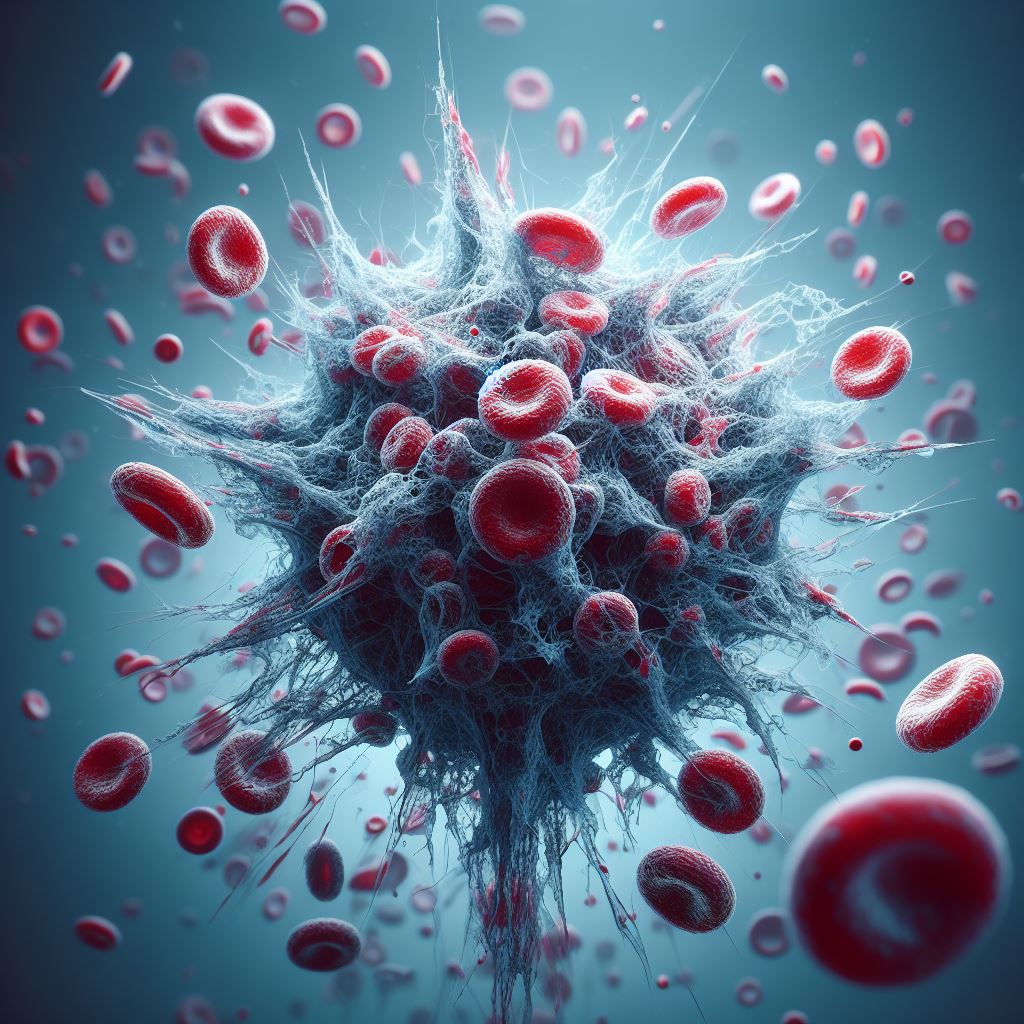
Aggressive blood malignancy is called acute myeloid leukaemia (AML). It is brought on by mutations in a multitude of genes that are acquired over an individual’s lifetime. The tumour suppressor gene TP53 is one of these genes that is crucial. TP53 typically aids in preventing the growth of tumours. Patients with blood cancer who have this gene altered, however, have a very bad prognosis since their mutations make them resistant to traditional chemotherapy drugs. As a result, much research is being done on novel therapeutic strategies, such as CAR (chimeric antigen receptor) T-cells, which have already shown promise in the treatment of other blood malignancies.
Professors Markus Manz and Steffen Boettcher of the University of Zurich (UZH) and the Department of Medical Oncology and Hematology at the University Hospital Zurich (USZ) are leading an international research team that has demonstrated that AML cells with TP53 mutations are also markedly more resistant to CAR T-cell therapy, a novel form of immunotherapy, than AML cells without the mutation.
The reason for the poorer effect of CAR T-cells with mutated TP53 is that these immune cells are exhausted more quickly and are therefore less active against the cancer cells
Steffen Boettcher, chief of service at USZ
Certain immune cells called T-cells are taken out of a patient’s blood and used in CAR T-cell therapy. Then, in the lab, these immune cells undergo genetic modification to create a large number of additional contact points (CARs) on their surface. After being reintroduced into the patient, the CAR T-cells can identify certain surface features on the tumor cells. This allows the CAR T-cells to target and destroy the cancer cells. Early-stage clinical studies are presently testing a variety of CAR T-cell products against AML.
The method by which mutated AML cells resist CAR T-cell immunotherapy was not the only thing the researchers looked at in their study; they also learned how to make CAR T-cells more resilient and how to take advantage of a weakness in TP53-mutant AML cells to overcome this resistance. They were able to significantly boost the efficacy of CAR T-cells against TP53-mutant AML cells to the point where there was no longer any therapeutic difference compared to non-mutant AML cells through additional pharmacological concomitant therapies or further genetic improvement of the CAR T-cells.
This proof-of-principle study shows that concurrent pharmacological therapies and genetically engineered CAR T-cells are promising strategies to develop more effective and tolerable immunotherapies for patients with TP53-mutant AML.
Markus Manz, head of clinic
Source: University of Zurich – UZH News
Journal Reference: Jan Mueller, Roman R Schimmer, et al. Targeting the mevalonate or Wnt pathways to overcome CAR T-cell resistance in TP53-mutant AML cells. EMBO Molecular Medicine. 14 March 2024. DOI: https://doi.org/10.1038/s44321-024-00024-2
Last Update: