The female reproductive system shows regular cyclic changes that may be calculated as periodic preparation for pregnancy and fertilization and in humans, the cycle is called the menstrual cycle, which occurred by the rupturing of the uterus lining.
The uterus lining comprises of perimetrium, which is the epithelial outer layer, the endometrium, which is the vascular layer and the myometrium, the muscular lining. As endometrium is the vascular layer its breakage leads to menstrual bleeding. The formation of the endometrium is regulated by the growth regulator, oestrogen, that activates the progesterone receptors in the endometrium there occurs a signalling cascade leading to the synthesis and storage of glycogen and blood vessel synthesis occurs.
In primate endometrium breaks with the breakage of the splanchnic artery and for humans, it is the spiral artery breakage that leads to menstrual bleeding. The length of the cycle can be an average that’s 28 days from the start of one menstrual period to the start of the next.
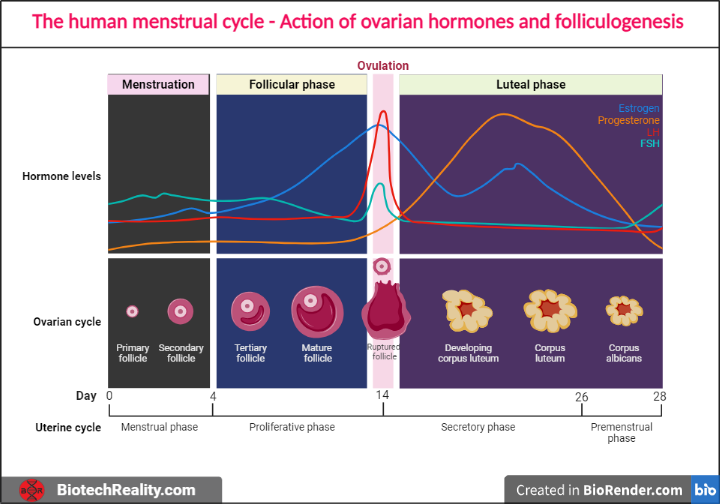
The menstrual cycle has four phases that are controlled by the release of various hormones and the phases are,
- Menstrual phase
- Proliferative phase
- Ovulatory phase
- Luteal phase
1. Menstrual phase
The menstrual phase refers to the first five days (1-5) of the menstrual cycle and it starts with the rupture of the endometrium when there is no fertilization (fusion of egg and sperm). During this phase, the level of oestrogen, as well as progesterone, decreases.
2. Proliferative phase
Represents the 6-13 days of a menstrual cycle. It is also known as the follicular phase as the maturation of the Graafian follicle occurs during this phase and the regeneration of the endometrium starts here. The two major hormones that are produced during this phase are the follicle-stimulating hormone (FSH) and luteinizing hormone (LH) and FSH activates the FSH receptors on the granulosa layer by binding on it, that in turn synthesise and activate oestrogen on the day 13.
3. Ovulatory phase
14th day of the menstrual cycle where the oestrogen gives positive feedback to the hypothalamus leading to the release of gonadotropin-releasing hormone (GnRH). GnRH acts on the anterior pituitary gland leading to an increased release of LH called the LH surge and LH binds to the LH receptors in the Graafian follicle. Thus, the Graafian follicle ruptures and leads to the release of the ovum it is termed ovulation.
4. Luteal Phase
This represents the 15-28 days of a menstrual cycle, where to the empty Graafian follicle or what can be termed as corpus hemorrhagic, the blood fills into it and later forms the corpus luteum. The corpus luteum is a temporary endocrine gland that produces the hormones, oestrogen and progesterone that will give negative feedback to the hypothalamus to down-regulate the release of FSH and LH.
The Corpus luteum ruptures if fertilization does not occur until the 28th day and becomes a scar tissue called corpus albicans. In higher organisms, the corpus luteum is ruptured by prostaglandins and the cycle continues.
FDA approved the initiatory oral pill treatment for Postpartum Depression (PPD)
Human chorionic gonadotropin (hCG), which stimulates the generation of oestrogen and progesterone and maintains the corpus luteum, is released by the growing embryo if fertilisation and implantation take place. These hormones assist maintain the uterine lining to support the developing embryo and stop subsequent ovulation.
It’s crucial to remember that hormone levels and their effects might differ between people and cycles. The menstrual cycle can also be affected by elements including stress, physical health issues, and lifestyle choices. The reproductive system is able to work effectively because of the complex coordination of these hormones, which controls the whole menstrual cycle.
Folliculogenesis
The process of follicle formation within the ovaries is called folliculogenesis. A developing egg (oocyte) is housed in a tiny, fluid-filled sac called a follicle in the ovaries. The growth and maturity of these follicles, which eventually results in ovulation and the possibility of fertilisation, depend heavily on the process of folliculogenesis.
- Primordial Follicles: The earliest stage of follicle formation, primordial follicles are seen in the ovaries even before a female is born. A single layer of flat cells surrounds the immature egg found inside each primordial follicle.
- Primary Follicles: Some primordial follicles are stimulated to continue developing under the influence of hormonal cues. The cells that are in close proximity to the egg begin to divide and form a layer of granulosa cells. The shift to primary follicles is signalled by this.
- Secondary Follicles: The granulosa cell layer thickens within secondary follicles, and the follicle begins to discharge fluid, creating the antrum, a hollow filled with fluid. The follicle is now known as an antral or secondary follicle as the antrum grows.
- Graafian Follicle: A prominent antral follicle emerges as a result of hormonal cues. This dominating follicle keeps expanding and getting a bigger antrum. The cumulus oophorus, a heap of granulosa cells that encircles the egg, also forms. The Graafian follicle is the name given to the mature dominant follicle.
- Ovulation: Ovulation is brought on by a spike in luteinizing hormone (LH), which happens in the middle of the menstrual cycle. When the Graafian follicle bursts, the mature egg and accompanying cumulus cells are released into the fallopian tube along with it. The ovulation process looks like this.
- Corpus Luteum: The corpus luteum is a tissue that develops in the ovary after ovulation from the leftover follicular cells. Progesterone is produced by the corpus luteum and aids in maintaining the uterine lining in anticipation of prospective embryo implantation.
- Corpus Albicans: The corpus luteum regresses and transforms into the corpus albicans, a white scar-like structure if fertilisation and implantation do not take place. As a result, hormone synthesis declines, resulting in the uterine lining falling out and menstruation.
The pituitary gland’s secretion of the hormones follicle-stimulating hormone (FSH) and luteinizing hormone (LH), as well as regional ovarian factors, carefully controls the process of folliculogenesis. A pool of follicles forms as a result of this complex process, with one follicle normally becoming dominant and going through ovulation throughout each menstrual cycle.
Image Source: BiorRender.com
Qualified CSIR - National Eligibility Test (NET), eligible for Assistant Professorship in any Indian university. Graduated from the University of Kerala with B.Sc. Botany and Biotechnology. Attained Post-Graduation in Biotechnology from the Kerala University of Fisheries and Ocean Science (KUFOS) with the fourth rank. Conducted various seminars and presentations. Experienced in ELISA, Blotting, and other Good Laboratory Practices. Attended a certificate course in Patent Analytics. Done 6 months of internship in ICMR - Vector Control Research Center, Puducherry. 3 years of tutoring experience.