A new compound created by researchers at Washington University School of Medicine in St. Louis successfully cures bacterial infections in mice, including those that can cause uncommon but potentially deadly “flesh-eating” disorders. The medicine in question has the potential to be the first in a completely new class of antibiotics, which would be a boon for doctors looking for more robust therapies for germs that are difficult to suppress with current drugs.
Their findings were published in the journal Science Advances.
For medics looking for efficient therapies against harmful microorganisms that are growing increasingly resistant to already existing medications, the discovery of a novel type of antibiotic would be excellent news.
All of the gram-positive bacteria that we’ve tested have been susceptible to that compound. That includes enterococci, staphylococci, streptococci, C. difficile, which are the major pathogenic bacteria types,
The compounds have broad-spectrum activity against numerous bacteria.
Michael Caparon, PhD
It is predicated on ring-fused 2-pyridone, a particular kind of chemical. Originally, Almqvist was tasked by Caparon and Hultgren with creating a substance that would stop bacterial films from adhering to the urethral catheter surface, which is a frequent source of UTIs linked to hospitals. It was a pleasant accident to find that the resultant chemical exhibited anti-infection effects against several types of bacteria.
The researchers gave the novel class of chemicals the name GmPcides (for gram-positive-icide). The authors have previously demonstrated that GmPcides can eradicate bacterial strains in petri dish tests. They chose to test it on necrotising soft-tissue infections in this most recent study because Caparon already had a functional animal model for these fast-spreading illnesses, which typically include numerous types of gram-positive bacteria. The most well-known of them, necrotising fasciitis, sometimes known as “flesh-eating disease,” can cause tissue destruction so rapidly that limb amputation is necessary to stop its spread. Flesh-eating sickness victims die in around 20% of cases.
The substance seemed to lessen the bacteria’s aggressiveness and, astonishingly, hasten the skin’s healing process after an infection.
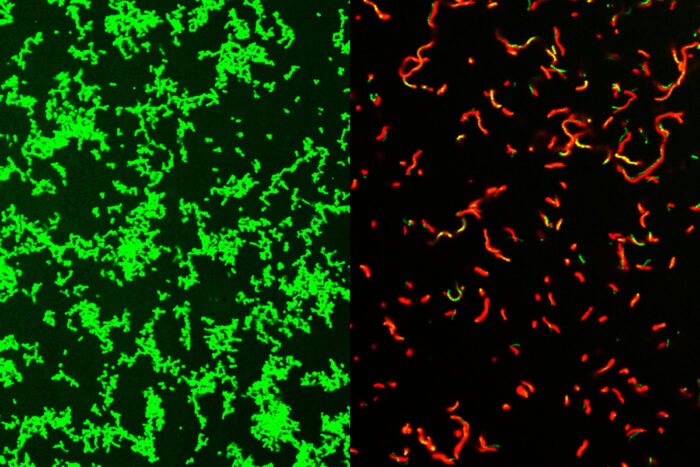
The method by which GmPcides manage to achieve all of this remains unclear, but microscopic analysis indicates that the treatment seems to have a major impact on the bacterial cell membranes, which are the germs’ outer layer.
The method by which GmPcides manage to achieve all of this remains unclear, but microscopic analysis indicates that the treatment seems to have a major impact on the bacterial cell membranes, which are the germs’ outer layer.
One of the jobs of a membrane is to exclude material from the outside,
We know that within five to ten minutes of treatment with GmPcide, the membranes start to become permeable and allow things that normally should be excluded to enter into the bacteria, which suggests that those membranes have been damaged.
Michael Caparon, PhD
This can impair the bacteria’s ability to carry out their own tasks, such as harming their host, and reduce their capacity to thwart the host’s immune system’s reaction to infections.
GmPcides not only work well against bacteria, but they also don’t seem to produce strains that are resistant to drugs. Few cells were detected in experiments aimed at producing resistant bacteria that could endure treatment and pass on their benefits to the following generation of bacteria.
Before GmPcides are likely to be seen at neighbourhood pharmacies, Caparon said, there is still a long way to go. In the hopes of working with a business that can oversee clinical trials and pharmaceutical development to possibly bring GmPcides to market, Caparon, Hultgren, and Almqvist have patented the compound used in the study and licensed it to QureTech Bio, a company in that own stock.
Also, Read| A discovery shows that lung repair after viral infections by a new population of macrophages
Hultgren claimed that treating unsolvable issues like antibiotic resistance requires the type of cooperative science that produced GmPcides.
Bacterial infections of every type are an important health problem, and they are increasingly becoming multidrug resistant and thus harder to treat,
Interdisciplinary science facilitates the integration of different fields of study that can lead to synergistic new ideas that have the potential to help patients.
Scott Hultgren, PhD
Source: Washington University of Medicine St. Louis – News
Journal Reference: Zou, Zongsen, et al. “Dihydrothiazolo Ring-fused 2-pyridone Antimicrobial Compounds Treat Streptococcus Pyogenes Skin and Soft Tissue Infection.” Science Advances, 2024, DOI: 10.1126/sciadv.adn7979.
Last Modified: