Researchers at Vanderbilt University Medical Centre have shown that while fever raises immune cell metabolism, proliferation, and activity, it also causes mitochondrial stress, DNA damage, and cell death in a specific subgroup of T cells.
Their findings were published in the journal Science Immunology.
The corresponding author of the current study, Jeff Rathmell, PhD, Cornelius Vanderbilt Professor of Immunobiology, said that the effects of fever temperatures on cells are a topic that has not received much research. According to him, the majority of studies on temperature that is now available is focused on agriculture and the effects of high temperatures on animals and crops. Animal models are difficult to adjust in a way that doesn’t stress them out, thus cells are usually maintained in labs at 37 degrees Celsius (98.6 degrees Fahrenheit), which is the temperature of human bodies.
Standard body temperature is not actually the temperature for most inflammatory processes, but few have really gone to the trouble to see what happens when you change the temperature.
Jeff Rathmell, PhD
For personal reasons, graduate student Darren Heintzman was intrigued by the effects of fevers: before to joining the Rathmell lab, his father suffered from an autoimmune condition that left him with a persistent fever for months at a time.
I started thinking about what an increased set point temperature like that might do. It was intriguing,
Darren Heintzman
Heintzman used 39 degrees Celsius, or around 102 degrees Fahrenheit, to cultivate immune system T cells. He discovered that heat boosted helper T cell metabolism, proliferation and inflammatory effector activity and reduced regulatory T cell suppressive ability.
If you think about a normal response to infection, it makes a lot of sense: You want effector (helper) T cells to be better at responding to the pathogen, and you want suppressor (regulatory) T cells to not suppress the immune response.
Darren Heintzman
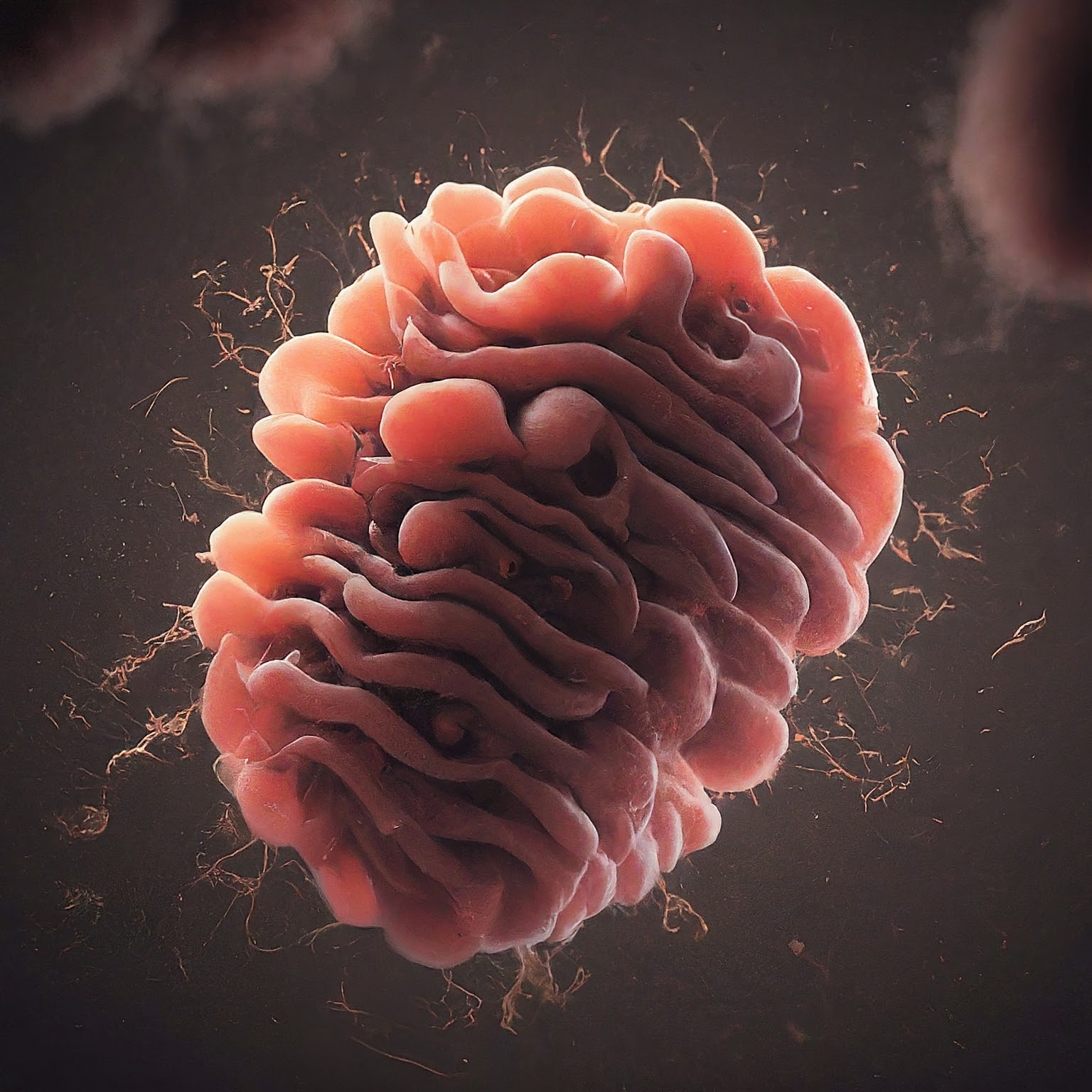
However, the researchers also found an unexpected finding: certain Th1 cells, a particular subtype of helper T cells, experienced DNA damage and mitochondrial stress. According to the researchers, the discovery was puzzling because Th1 cells are implicated in conditions like viral infections when fever is frequently present. Why would the cells die that are essential for battling the infection?
Only a small percentage of Th1 cells die, the researchers found; the remaining Th1 cells adapt, alter their mitochondria, and become more resilient to stress.
There’s a wave of stress, and some of the cells die, but the ones that adapt and survive are better — they proliferate more and make more cytokine (immune signaling molecules)
Jeff Rathmell, PhD
The molecular processes behind the cell’s reaction to fever temperatures were clarified by Heintzman. He discovered that the energy-producing mitochondrial protein complex known as electron transport chain complex 1 (ETC1) was quickly harmed by heat. The loss of ETC1 activated signalling pathways that resulted in damage to DNA and the activation of the tumour suppressor protein p53, which either initiates cell death or facilitates DNA repair in order to preserve the integrity of the genome. When it came to defective ETC1, Th1 cells were more susceptible than other T cell subtypes.
The researchers further supported the molecular signalling route they established when they discovered Th1 cells with comparable alterations in sequencing databases for samples from individuals with rheumatoid arthritis and Crohn’s disease.
We think this response is a fundamental way that cells can sense heat and respond to stress,” Rathmell said.
Temperature varies across tissues and changes all the time, and we don’t really know what it does. If temperature changes shift the way cells are forced to do metabolism because of ETC1, that’s going to have a big impact. This is fundamental textbook kind of stuff.
Jeffrey Rathmell, PhD
Also, Read| Genetic risk-factor overlap between Alzheimer’s disease and vascular dementias
According to the research, heat can cause mutations when cells that experience mitochondrial stress fail to adequately repair DNA damage or perish.
Chronic inflammation with sustained periods of elevated tissue temperatures could explain how some cells become tumorigenic.
Darren Heintzman
Source: VUMC News
Journal Reference: Heintzman, Darren R., et al. “Subset-specific Mitochondrial Stress and DNA Damage Shape T Cell Responses to Fever and Inflammation.” Science Immunology, 2024, DOI: https://doi.org/10.1126/sciimmunol.adp3475.
Last Modified: