To an extent previously believed to be feasible only by neutralizing antibodies, researchers from Singapore General Hospital and Duke-NUS Medical School have shown that T cells white blood cells that may eliminate dangerous pathogens can totally prevent viral infection. Their results, which have been empirically demonstrated for the first time in human research, fundamentally alter our knowledge of how the immune system functions and open the door to the development of more potent vaccinations.
Neutralizing antibodies, which are proteins that stop viruses from entering cells, have long been thought of by scientists as the best defense against viral illnesses. By binding to viruses, these antibodies stop them from infecting cells, ensuring that no signs of infection are detected in clinical or laboratory settings. Sterilizing immunity is the term used to describe this degree of defense.
Their findings were published in the journal Nature Microbiology.
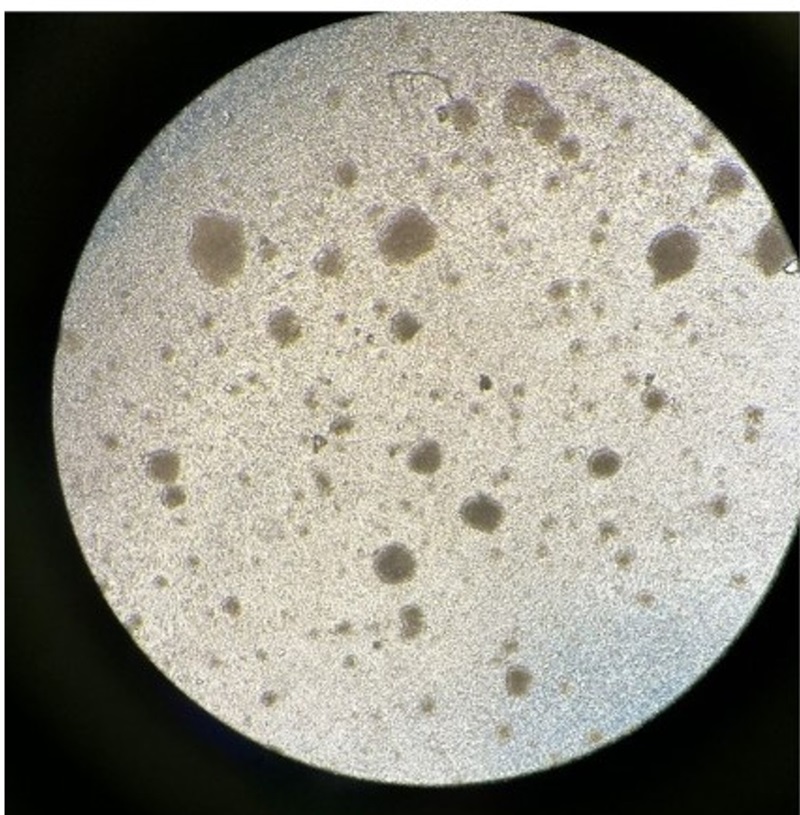
Researchers used a cross-vaccination strategy in the trial, which involved 33 healthy adult volunteers between the ages of 21 and 45. They gave the participants a live-attenuated yellow fever vaccine, followed by a challenge with a weakened Japanese encephalitis virus 28 days later, and vice versa. The viruses that cause Japanese encephalitis and yellow fever share genetic similarities. Although the reduced strains could not infect the volunteers, they were enough to produce the immunological response required for protection, moderate symptoms, and detectable virus levels in the blood. From March 30, 2023, to October 31, 2023, the study was carried out at the SingHealth Investigational Medicine Unit in Singapore.
Inoculation with either vaccine produces T cells that are effective against both viruses, but it also stimulates the production of neutralizing antibodies that are ineffective against the virus used in the human challenge study. This is because the Japanese encephalitis vaccine was developed using the foundation of the yellow fever vaccine. This made it possible for the researchers to evaluate the T-cells’ ability to manage the infection without the aid of neutralizing antibodies.
The findings demonstrated that the Japanese encephalitis vaccine virus challenge infection was managed by T cells derived from yellow fever vaccination, which decreased viral loads and antibody production. Additionally, following immunization, when levels are sufficiently high.
We found that T cells can serve as the first line of defence, not just a supportive element in protecting us from acute viral diseases. These findings challenge the current paradigm that antibodies are absolutely vital for protection against acute viral infection. Measuring antibodies alone without considering T cells could underestimate herd immunity—when sufficient numbers of individuals in a population are already protected against specific viruses either through vaccination or previous infections—which is one of the considerations in developing policies on vaccine dosage and frequency.
Ooi Eng Eong
Historically, producing high antibody levels has been the top priority in vaccine research. This strategy could not only reduce the effectiveness of vaccinations but also make it more difficult to fight against variations that evade T cells but not antibodies.
We need to rethink how we design and develop vaccines. Vaccines that generate high levels of antibodies do not necessarily generate high levels of T cells. Development of vaccines must incorporate the viral components that T cells recognise and react against. Indeed, our findings may explain why some vaccines offer better protection against viruses when they are able to trigger a broader T cell response.
Shirin Kalimuddin
Also Read: New Skeletal Tissue Advances Regenerative Medicine Potential
The study findings encourage us to integrate both antibody and T-cell responses to create more effective and comprehensive vaccines. By understanding the unique roles T cells play, especially in viruses like yellow fever, dengue and Zika, all of which are from the same family and could pose a public health threat in Singapore due to Aedes mosquito transmission, we can develop vaccines that target a wider range of viral strains and mutations to control such untreatable diseases.
Patrick Tan
The researchers’ next goal is to investigate why some people react to immunization with more T cells than others. Duke-NUS is a biomedical research powerhouse and a leader in medical education. It combines translational knowledge with basic scientific research to better understand human biological systems and create new vaccines and treatments for common diseases that affect millions of people in Singapore and Asia.
Source: Duke NUS – News
Journal Reference: Kalimuddin, Shirin, et al. “Vaccine-induced T Cell Responses Control Orthoflavivirus Challenge Infection Without Neutralizing Antibodies in Humans.” Nature Microbiology, 2025, pp. 1-14, DOI: https://doi.org/10.1038/s41564-024-01903-7.
Last Modified: