According to new research funded by the National Institutes of Health (NIH) and published today in the journal Science, a single alteration in the protein on the surface of the highly pathogenic avian influenza (HPAI) H5N1 influenza virus that is presently circulating in U.S. dairy cows may make it easier for the virus to spread among humans. The study’s findings support the necessity of ongoing, careful surveillance and monitoring of HPAI H5N1 for any genetic alterations that can increase the virus’s human transmissibility.
Although it is unknown if the current strains of the bovine (cow) H5N1 virus may spread to humans, illnesses have happened to people who have come into contact with infected wild birds, poultry, dairy cows, and other mammals. In order to better understand natural viral genetic alterations and their potential effects on transmissibility, researchers have been studying the H5N1 virus for years as part of pandemic preparedness efforts.
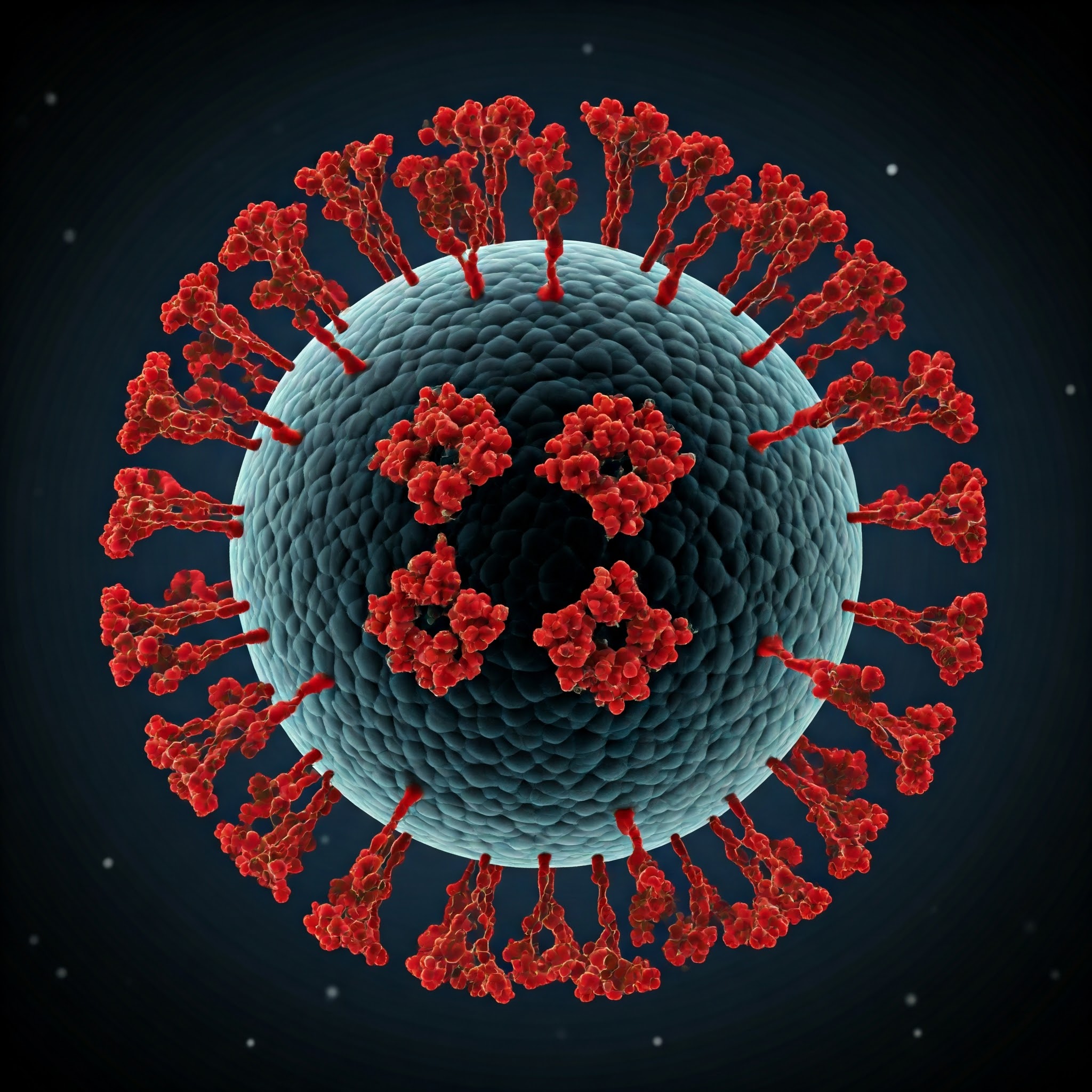
Influenza viruses need a surface viral protein known as hemagglutinin (HA) to adhere to cells. To infect cells, the HA attaches itself to receptors for sugar (glycan) molecules. Because the human upper respiratory tract lacks the avian-type cell receptors present in birds, avian (bird) influenza viruses, such as H5N1, have not frequently infected humans. Scientists are worried that viruses may develop the capacity to infect humans and spread among them if they learn to identify human-type cell receptors in the upper airways.
Researchers at Scripps Research tested the effects of changes in the HA gene sequence on the binding of that protein with avian versus human-type cell receptors using the H5N1 strain that was obtained from the first human infection in the United States with the bovine strain 2.3.4.4b (A/Texas/37/2024). The researchers inserted a number of mutations into the viral HA protein that had previously been seen to arise naturally. They discovered that one of these mutations, Q226L, enhanced the protein’s capacity to bind to receptors normally present on human cells, particularly when accompanied by another mutation. Crucially, the scientists did not produce or test an infectious virus in its whole; instead, they merely inserted the genetic alterations into the HA surface protein.
Also Read: Brain Tumors Attract Killer T Cells via Molecular Zip Code
The authors point out that the experimental discovery of the Q226L mutation by itself does not indicate that HPAI H5N1 is about to unleash a massive pandemic. It would probably take more genetic alterations for the virus to spread from person to person. The results highlight the significance of ongoing outbreak control efforts and ongoing genomic surveillance to keep an eye out for the emergence of HPAI H5N1 genetic changes and preserve public health preparedness, especially in light of the increasing number of H5N1 human cases that have been linked to direct contact with infected animals.
Source: National Institutes of Health – News
Journal Reference: Lin, Hui, et al. “A Single Mutation in Bovine Influenza H5N1 Hemagglutinin Switches Specificity to Human Receptors.” Science, 2024, DOI: 10.1126/science.adt0180.
Last Modified: